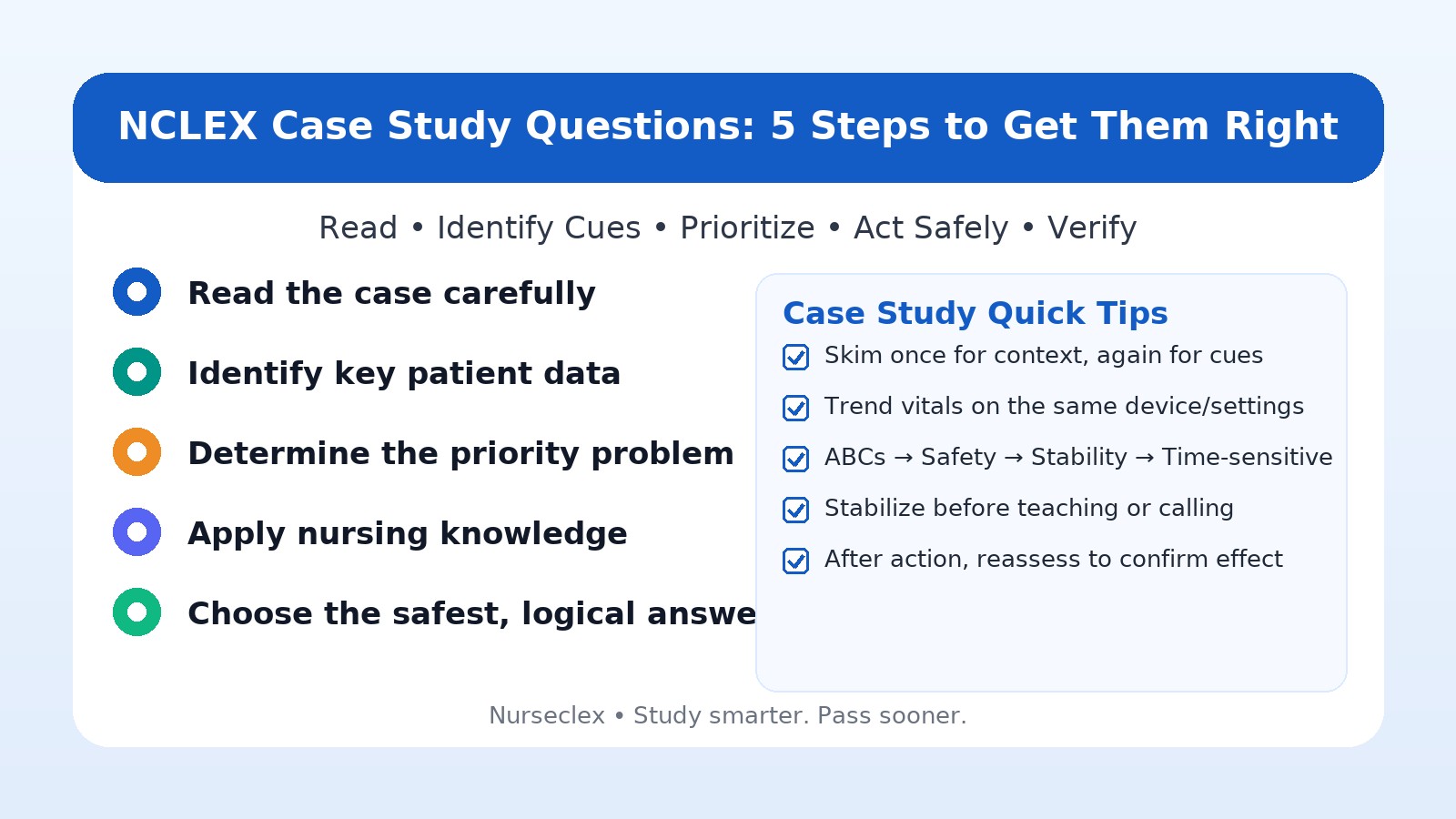
Preparing for the NCLEX can feel overwhelming—especially when you hit NCLEX case study questions. These items test how you apply knowledge, recognize cues, analyze data, and use clinical judgment—just like real practice. The good news: a clear, repeatable method makes them manageable.
Below is a five-step approach to break any case into actions you can execute fast.
Quick take: the 5 steps
-
Read the case carefully
-
Identify key patient data
-
Determine the priority problem
-
Apply nursing knowledge
-
Choose the safest, most logical answer
Step 1: Read the case carefully
Resist the urge to skim. Case sets include extra details by design.
Do this:
-
Note age, history, setting (ED/med-surg/post-op), and presenting complaint.
-
Scan vitals, labs, diagnostics, meds, and recent changes.
-
Ask yourself: What is this case likely about—oxygenation, perfusion, neuro, infection, or metabolic?
Practice CAT-style pacing: see CAT Simulation
Step 2: Identify key patient data
Separate signal from noise. Focus on what matters for safety now.
Pull out:
-
Abnormal vitals (e.g., SpO₂ ≤ 90%, RR ↑, MAP < 65).
-
Critical labs (e.g., K⁺ 6.2, troponin ↑, glucose extremes).
-
Red-flag symptoms (new confusion, unilateral neuro deficits, severe dyspnea).
-
Device/setting details (same device and flow when trending O₂).
Sharpen cue recognition and ranking: Analysis & Prioritization
Step 3: Determine the priority problem
Choose the problem that threatens life or safety first.
Use frameworks:
-
ABCs → Safety → Stability → Time-sensitive
-
Maslow (physiological before psychosocial)
-
Stable vs. unstable (trending worse = unstable)
Examples:
-
SOB + SpO₂ 88% on 2 L NC → Oxygenation first.
-
New unilateral weakness + slurred speech → Neuro perfusion first.
-
Urine output 20 mL/hr + cool, clammy skin on vasopressors → Perfusion first.
Step 4: Apply nursing knowledge
Pick actions that address the priority safely and within scope.
Ask:
-
What is the safest first intervention?
-
What’s RN-only vs. what can be delegated?
-
What will I monitor to confirm effect and catch complications?
Examples:
-
SpO₂ 82% on 2 L NC → escalate oxygen per protocol (device/flow) + high-Fowler’s.
-
New IV heparin → check aPTT per protocol and have protamine available.
-
Severe preeclampsia on MgSO₄ → seizure precautions + monitor RR, DTRs, UO for toxicity.
Step 5: Choose the safest, most logical answer
When you hit the choices:
Do this first:
-
Eliminate unsafe and out-of-scope options.
-
Drop teaching if the patient is unstable (stabilize before education).
-
Prefer specific, timely rationales (safety, protocol targets, toxicity monitoring) over vague ones.
If two look right: pick the safer first action that directly addresses the priority problem. After action, ask: What will I reassess (e.g., SpO₂ ≥ 92%, RR improving, neuro status)?
Common mistakes (and easy fixes)
-
Skimming the stem → Read once for context, again for cues.
-
Chasing noise → Filter to abnormal vitals/labs and red flags.
-
Teaching too soon → Stabilize first.
-
Scope errors → Keep assessments/initial teaching/evaluation with the RN.
-
Ignoring trends → Compare same device and settings before calling it a trend.
Build consistency with mixed practice sets: QBank Hub
Mini-drills (one-liners)
-
O₂ downtrend on same device: escalate oxygen device/flow + high-Fowler’s.
-
Heparin infusion started: check aPTT per protocol; monitor bleeding.
-
New unequal pupils post-injury: protect airway, notify STAT, prep imaging.
-
K⁺ 6.5 with ECG changes: stabilize myocardium (calcium gluconate) while shifting K⁺ as ordered.
Round out your prep: Therapeutic Communication
Final thoughts
NCLEX case study questions reward disciplined thinking. Read carefully, pull the right cues, set the correct priority, choose the safest first action, and verify your result. Repeat this method, and your clinical judgment—and confidence—will climb.
Next step: Run a 10-item case set, log misses by content vs strategy, and retest within 24–72 hours. You’ve got this.